How to Regulate Cortisol Levels – Mastering Your Stress
Cortisol, often referred to as the “stress hormone,” plays a pivotal role in regulating numerous bodily functions. To truly appreciate its impact on our overall health and well-being, it’s essential to delve into the specifics of its functions, the implications of imbalance, and how to regulate cortisol levels.
How To Regulate Cortisol Levels
Adrenal glands on top of our kidneys create the steroid hormone cortisone. The hypothalamic-pituitary-adrenal (HPA) axis, a complex interplay of signals and reactions, principally regulates the production and release of this hormone. Let’s learn how to regulate cortisol levels.
The Regulation of Cortisol
Cortisol serves several crucial functions in the body:
- Stress Response: It plays an integral part in the body’s ‘fight or flight’ stress response. During moments of stress, cortisol levels surge to prepare the body for potential threats.
- Metabolism Regulation: Cortisol helps regulate metabolism by determining the utilization of carbohydrates, fats, and proteins, thereby influencing body weight.
- Immune Function: It modulates the immune system’s response, acting as a potent anti-inflammatory agent during illness or injury.
- Blood Pressure Regulation: Cortisol helps maintain blood pressure by increasing the sensitivity of blood vessels to epinephrine and norepinephrine. You can do self-monitoring at home. Here’s a link! https://amzn.to/4j9hQNh
Imbalance in Cortisol

Despite cortisol’s necessity, an imbalance, either too high or too low, leads to significant health issues. Never rule out a good exercise routine. Exercise is a natural stress reliever. Just 20 minutes a day works fine. Too much cortisol is not a good sign.
Hypercortisolism (High Cortisol)
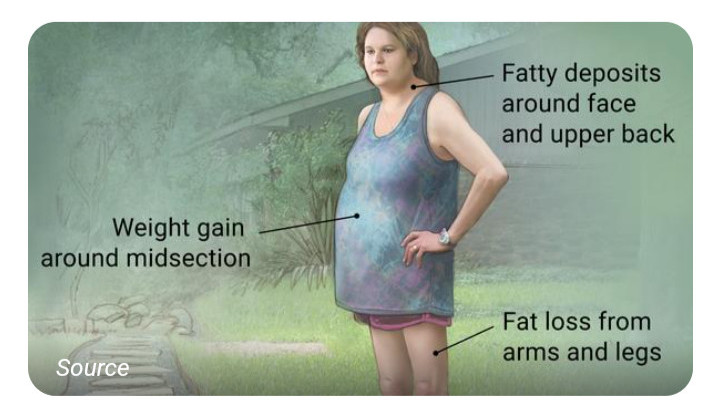
Chronic stress or disorders like Cushing’s syndrome lead to an overproduction of cortisol. Hypercortisolism is a condition that has been associated with a number of medical conditions, including:
- Weight gain, particularly around the abdomen
- High blood pressure
- Diabetes
- Osteoporosis
- Anxiety and depression
- Impaired cognitive function
Treatment Options
When it comes to treating high cortisol levels, the causes, symptoms, and individual health profiles dictate the course of action. The world of medicine offers a plethora of options to manage and treat high cortisol levels. Among these, certain categories of drugs are more prevalent and are often recommended by medical professionals. Adrenal Enzyme Inhibitors have unique properties.
Adrenal Enzyme Inhibitors
One of the most common medications used is adrenal enzyme inhibitors. As their name implies, these inhibitors work by blocking the activity of certain enzymes in the adrenal glands involved in the production of cortisol, thereby reducing its levels. This brings us to the topic of adrenolytic agents.
Adrenolytic Agents
Adrenolytic agents, another class of drugs, function by destroying parts of the adrenal glands to decrease cortisol production. Simultaneously, glucocorticoid-receptor antagonists work slightly differently, blocking the cortisol receptors in body cells and thereby reducing the effects of excessive cortisol. Of course, there are other pharmacological options.
Pharmacological Options

Among these, adrenal enzyme inhibitors are frequently prescribed due to their efficiency and fewer side effects. Other potential pharmacological options include drugs like metyrapone and mitotane, which act by suppressing the adrenal gland’s ability to produce cortisol. However, it is recommended that you incorporate lifestyle changes.
Lifestyle Modifications to Curb Cortisol Levels
Chronic stress, a prevailing issue in today’s fast-paced world, is a significant contributor to escalating cortisol levels. Lack of physical activity is a concern.
Physical Activity Reduces Stress
Physical activity is a potent stress reducer. Regular exercise, be it a high-intensity workout or a relaxing walk, significantly helps lower cortisol levels. Journaling is another effective method. It aids in processing thoughts, thereby reducing the stress burden on the mind. Consider mindfulness as a viable option.
Mindfulness and Medication
In addition, mindfulness or meditation practices can play a critical role in managing cortisol. These techniques help to cultivate a state of relaxation, promoting mental clarity and stress reduction, which in turn aids in effective cortisol regulation. However, never rule out clinical or lifestyle approaches.
Combining Clinical and Lifestyle Approaches
Addressing high cortisol levels is not just about medications or surgery; it’s about integrating these treatments with lifestyle changes that sustain cortisol at optimal levels. A comprehensive approach involving medical professionals, therapeutic interventions, and personalized stress management strategies is the ideal path toward effective cortisol regulation.
Hypocortisolism (Low Cortisol)

On the other hand, insufficient cortisol production, known as hypocortisolism, results from Addison’s disease or secondary adrenal insufficiency. Symptoms include:
- Fatigue
- Weight loss
- Low blood pressure
- Abdominal pain
- Darkened patches of skin
Treatment for Low Cortisol
Treating low cortisol typically involves hormonal replacement therapy, which aims to replenish the deficit of cortisol in the body and thereby maintain a healthy hormonal balance.
The most commonly prescribed medication for this purpose is hydrocortisone, a synthetic glucocorticoid. Hydrocortisone mimics the function of natural cortisol, helping regulate the body’s metabolism and immune response, and maintain proper blood pressure. Having the right dosage and frequency is quintessential.
Dosage and Frequency for Low Cortisol
However, the dosage and frequency of administration must be carefully calibrated to align with the body’s natural rhythm of cortisol production. Too high a dose leads to symptoms of hypercortisolism, whereas too low a dose may not adequately manage the symptoms of hypocortisolism. Other medications such as flurocortisone are also helpful.
Fludrocortisone
In certain cases, fludrocortisone may also be prescribed. This medication serves to replace aldosterone, another hormone produced by the adrenal glands, which often gets impacted when cortisol levels are low.

While medication serves as a critical component in the management of low cortisol levels, lifestyle modifications also play a crucial role. Follow-ups and medication adjustments are extremely important.
Regular Follow-ups and Medication Adjustment
Scheduled check-ups with your healthcare provider are paramount for those dealing with hypocortisolism. This allows the doctor to adjust the medication dosage as necessary, monitor the progress of treatment, and manage any potential side effects.
Stress Management
Given that cortisol plays a crucial role in the body’s stress response, individuals with low cortisol levels find it more challenging to cope with stress. Incorporating stress-management techniques, such as regular exercise, deep breathing, yoga, and mindfulness meditation, helps manage the physiological response to stress.
Diet and Nutrition
Adopting a balanced, nutrient-rich diet is essential. Consuming adequate salt is particularly crucial for those prescribed with fludrocortisone, as this medication increases the body’s salt loss.
Medical Alert Identification
Wearing medical alert identification is a life-saver in emergency situations. In instances of acute adrenal crisis – a severe condition that occurs in people with hypocortisolism – immediate medical attention is needed, and identification expedites this process. Let’s dive into another example of elevated cortisol level- Cushing’s Syndrome.
Cushing’s Syndrome
Dwelling on the subject of cortisol imbalance, it’s essential to focus on one of the most common conditions linked with this anomaly: Cushing’s syndrome. Characterized by an overabundance of cortisol in the body, understanding Cushing’s syndrome involves analyzing its causes, recognizing its symptoms, and exploring the various treatment options available.
Understanding Cushing’s Syndrome
Although it can happen at any age, adults between the ages of 20 and 50 are the most frequently diagnosed. Let’s explore the causes of this condition.
The Causes
Cushing’s syndrome is caused by various factors, though they all result in the overproduction of cortisol. The primary causes include:
Pituitary Adenomas: This is the most common cause, leading to what’s known as Cushing’s disease. Benign tumors in the pituitary gland produce excess amounts of adrenocorticotropic hormone (ACTH), which in turn stimulates the adrenal glands to produce more cortisol.
Ectopic ACTH Syndrome: Certain types of tumors, such as lung or pancreatic tumors, produce ACTH, resulting in an overproduction of cortisol.
Adrenal Gland Tumors: Occasionally, benign or malignant tumors in the adrenal glands themselves lead to an overproduction of cortisol.
Long-term use of Corticosteroid Medications: This is known as iatrogenic Cushing’s syndrome. Corticosteroids, used for conditions like asthma and rheumatoid arthritis, lead to elevated cortisol levels if used in high doses over a long period. Here are the symptoms to look out for.
The Symptoms
The symptoms of Cushing’s syndrome are quite varied and may include:
- Weight gain, especially around the abdomen and face (creating a “moon face” appearance)
- Purple or pink stretch marks on the skin
- Thin skin that bruises easily
- Excess body and facial hair growth in women
- Irregular menstrual periods in women and decreased fertility in men
- High blood pressure and blood sugar levels
- Fatigue and muscle weakness
- Cognitive difficulties, anxiety, and depression
Diagnostic Measures for Cushing’s Syndrome
Diagnosing Cushing’s syndrome is extremely complex, as its symptoms often overlap with other conditions. Medical professionals typically rely on a combination of urine and blood tests and saliva tests taken at night when cortisol levels should be low. Anomalies in these results may indicate Cushing’s syndrome. Further imaging tests, such as CT scans or MRIs, help locate the presence of any tumors.
Treating Cushing’s Syndrome
Once diagnosed, treatment strategies focus on reducing the high cortisol levels. The approach largely depends on the underlying cause of the syndrome.
- Surgery: If a tumor is the source of the problem, as is often the case, the first line of treatment typically involves surgically removing it.
- Radiation Therapy: This is utilized if surgery isn’t an option or if some of the tumor remains post-surgery.
- Medications: Drugs help control cortisol production or block its effects. These are often used if surgery and radiation aren’t viable options or as a short-term measure to control symptoms before surgery.
Conclusion: A Balancing Act
Cortisol plays an integral part in our body’s functioning, and maintaining its balance is crucial for optimal health. Implementing stress-reducing practices and leading a balanced lifestyle contributes significantly towards achieving this balance. However, should symptoms persist, seeking professional medical advice is paramount.
Founder & CEO
(w) mybluegenes.com
(e) rachele@mybluegenes.com





As someone new to the topic of cortisol and its regulation, I found this article very informative and comprehensive. I can see how important it is to maintain cortisol levels for overall health and well-being. My experience with the topic is limited, but I am interested in learning more.
One thing that caught my attention is the mention of “Adrenolytic Agents” as a class of drugs that function by destroying parts of the adrenal glands to decrease cortisol production. This sounds like a very drastic measure. I wonder if there are any potential risks or side effects associated with using such agents. Are there alternative methods or treatments that are less invasive but still effective in regulating cortisol levels?
I also noticed that the article briefly mentioned “fludrocortisone” as a medication used to replace aldosterone, another hormone produced by the adrenal glands. Could you provide more details on how this hormone replacement therapy works for individuals with low cortisol levels? And are there any specific lifestyle modifications or dietary considerations that are important to follow while on such medication?
Lastly, I’m curious about Cushing’s syndrome, which is described as a condition where the body is exposed to high levels of cortisol over an extended period. How common is this syndrome, and are there any early warning signs that someone might be developing it? Additionally, how do medical professionals distinguish Cushing’s syndrome from other conditions with overlapping symptoms, and what are the available treatment options for managing this condition effectively?
Hi there, Skamalka.
Thank you for taking time out of your busy schedule to read and make generous comments on my article relating to regulating cortisol. There are so any of us dealing with stress nowadays. This is why it is so important to make sure that you pay a visit with you primary care physician on a regular basis. They already have your personal medical history and can give you s advice.
Not every one needs to to have the adrenolytic drugs. Yes, there are side effects that you need to be aware of. I am not a doctor but I am passionate about keeping my audience up to date on things important to there health and overall well-being. Although I am very passionate about health issues and I love doing research, I still advise each individual to talk to their medical expert for further information. My information is to point you in he right direction. I cannot provide legal or medical advice. However, I love that you very inquisitive about the information that is being imparted to you.
Rachele
Thanks for sharing the bright and colorful food groups Your blog is very informative .
Hi there, Lamatha.
Thank you for stopping by to have a dialogue about how to regulate our stress levels by partaking of healthy, colorful foods of every hue. I must admit, the transition to a healthier lifestyle has not been easy. I finally decided to have a better relationship with food. It has been a wonderful journey. We must give these bodies the nourishment they deserve, especially as affiliate marketers.
Rachele