Who Can Get Sickle Cell Anemia – A Modern Day Solution
The acronym CRISPR/Cas9 stands for clustered regularly interspaced short palindromic repeats. What a tongue-twister, right? Are you also wondering who can get Sickle Cell Anemia? If so, you’re in the right place at the right time.
Who Can Get Sickle Cell Anemia?
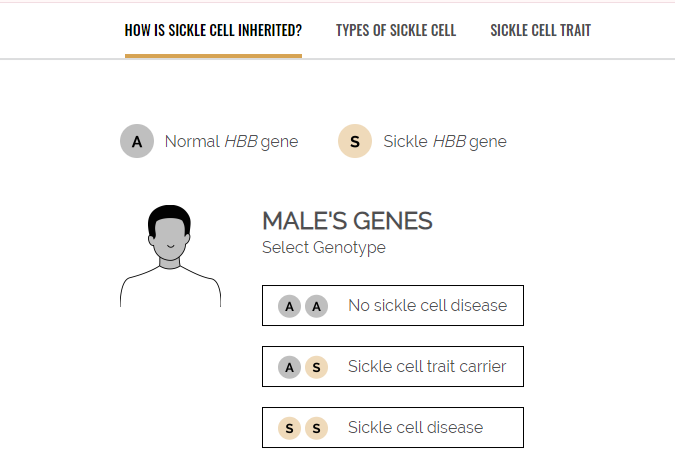
This disease does not affect everyone. Those born with a genetic predisposition are among those who can get sickle cell anemia. If you want to grasp the potential of CRISPR/Cas9 for curing sickle cell disease, you first need to understand the fundamentals of the condition itself.
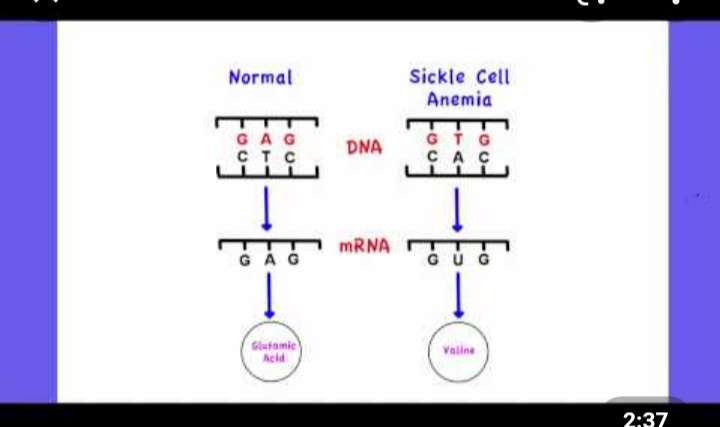
Sickle cell disease is a genetic disorder that affects hemoglobin, the molecule in red blood cells that delivers oxygen to cells throughout the body.
In contrast to popular opinion,sickle cell disease is not only found in African Americans. People from othe cultural backgrounds also have the sickle cell gene. In fact, here are a few statistics.
Sickle Cell Anemia may be found in:
- SCD affects approximately 100,000 Americans.
- SCD occurs among about 1 out of every 365 Black or African-American births.
- SCD occurs among about 1 out of every 16,300 Hispanic-American births.
- About 1 in 13 Black or African-American babies is born with sickle cell trait (SCT).
Due to a mutation in the hemoglobin gene, individuals with this disease have red blood cells that become rigid and shaped like a crescent, or sickle. This abnormal shape cause the cells to get stuck in blood vessels, leading to pain, infections, stroke, and cumulative organ damage over time.
The impact of sickle cell disease extends beyond the individual; it puts a significant strain on healthcare systems too. Many patients require frequent hospitalizations and ongoing treatment to manage the condition, leading to high medical costs and substantial use of resources.
The Girl With Sickle Cell Anemia
In high school, one of my classmates had sickle cell anemia. This was the first time I’ve ever heard of this word. However, she was never shy about saying that she had this disease. The one thing I do remember is that she was thin and lanky, her eyes seems to have a yellow tint, and she was absent a lot.
Signs and Symptoms of Sickle Cell
Sickle cell anemia is a genetic blood disorder characterized by the production of abnormal hemoglobin, known as hemoglobin S, which causes red blood cells to become rigid, sticky, and shaped like sickles or crescent moons.
These abnormal cells block blood flow, leading to pain and other serious problems such as infection, acute chest syndrome, and stroke. The signs and symptoms of sickle cell anemia vary and may range from mild to severe.
They typically begin in early childhood, but the age at which they first appear varies. To check to see if you may be susceptible, use a DNA. It is that simple.
Here are some common signs and symptoms:
1. Anemia:
The sickle cells break apart more easily and die sooner than normal red blood cells, leading to a shortage of red blood cells (anemia), causing fatigue and pallor.
2. Pain crises (sickle cell crisis):
Periodic episodes of pain, called pain crises, are a hallmark of sickle cell anemia. Pain occurs when sickled red blood cells block blood flow through tiny blood vessels to your chest, abdomen, and joints. Pain can also occur in your bones.
3. Swelling of hands and feet:
The swelling is caused by sickle-shaped red blood cells blocking blood flow to the hands and feet.
4. Frequent infections:
Sickle cells damage the spleen, an organ that fights infection, making patients more vulnerable to infections. Doctors commonly give infants and children with sickle cell anemia vaccinations and antibiotics to prevent potentially life-threatening infections, such as pneumonia.
5. Delayed growth or puberty:
A shortage of healthy red blood cells slows growth in infants and children and delay puberty in teenagers.
6. Vision problems:
Tiny blood vessels that supply your eyes may become plugged with sickle cells. This damages the retina and leads to vision problems.
Sickle cell anemia is usually detected at an early age through newborn screening programs. In the United States and many other countries, newborn screening tests check for sickle cell anemia along with other common conditions.
This test is typically done before the baby leaves the hospital after birth. If sickle cell anemia is detected, further tests will be done to confirm the diagnosis.

Early detection and treatment are crucial for managing symptoms and reducing the risk of complications associated with the disease. Treatment includes medications to reduce pain and prevent complications, blood transfusions, and other interventions to manage symptoms and maintain health.
Current treatments for sickle cell disease include blood transfusions and medications that reduce pain and prevent complications. However, these interventions often come with risks and side effects, and they don’t cure the disease.
That’s where gene editing, and particularly CRISPR/Cas9 technology, enters the picture, offering not just management but the potential for a permanent cure. I’m going to walk you through how this technology works and its incredible promise in the upcoming section.
CRISPR/Cas9: A Revolutionary Approach
If you’re curious about how we’re harnessing advanced science to tackle genetic disorders like sickle cell disease, CRISPR/Cas9 is where you should look. I’m going to let you in on why this gene-editing technology is such a game-changer.
Now, what exactly is CRISPR/Cas9? In a nutshell, it’s a cutting-edge tool that scientists use to edit the DNA of organisms with incredible precision. Think of it as a molecular pair of scissors that cut and paste genetic material. DNA is so fascinating, In fact, it’s easier than ever to find out about your own DNA.
To understand how CRISPR/Cas9 revolutionizes the treatment of sickle cell disease, it’s crucial to grasp how it targets the root cause. The disease stems from a single mutation in the hemoglobin gene. CRISPR/Cas9 goes straight to this defective gene, snip it out, and replace or repair it.
Why is this a big deal? Traditional treatments like bone marrow transplants carry risks and limitations, and gene therapy is complex and expensive. CRISPR/Cas9 offers a more precise and potentially cost-effective strategy.
And the real clincher? It’s not just theoretical. I’m talking about real-world instances where this technology has successfully edited genes in sickle cell patients to alleviate their symptoms.
In my opinion, the beauty of CRISPR/Cas9 lies not just in its precision, but also in its versatility. It has the potential to treat not only sickle cell disease but a vast array of genetic conditions. This isn’t just about cutting-edge science; it’s about real hope for millions of people worldwide.
Choose something that resonates with you, because the evidence is mounting: CRISPR/Cas9 is shaping up as our next big leap in medicine. And as we move on, you’ll learn about the ongoing clinical trials that are bringing us closer to a sustainable cure for sickle cell disease, pushing the boundaries of what CRISPR/Cas9 can achieve.

Clinical Trials and Research
The road to finding a cure for sickle cell disease via CRISPR/Cas9 gene editing is paved with rigorous clinical trials and extensive research. Clinical trials are essential in establishing the treatment’s safety and efficacy. Major research facilities around the world are undertaking these trials, offering a beacon of hope for patients.
On the ethical front, gene editing raises paramount questions. The idea of altering an individual’s genetic makeup carries implications not only for that person but potentially for future generations. Researchers, ethicists, and policymakers are working to address these concerns, ensuring that CRISPR/Cas9 is used responsibly.
Ensuring safety is at the heart of the research. Side effects, unforeseen consequences, and long-term impacts of gene editing are under strict scrutiny. Regulatory bodies, such as the FDA in the United States, thoroughly review all findings from clinical trials before approving any new treatment.
Looking to the horizon, the implications of this research are vast. Beyond just sickle cell, CRISPR/Cas9 has the potential to address a multitude of genetic conditions. Its advent heralds a new era of medicine where genetic disorders are corrected at their root.
Frequently Asked Questions
I’m going to address some of the common questions you might have about the CRISPR/Cas9 technology, especially as it relates to sickle cell disease.
Is CRISPR/Cas9 gene editing safe for treating sickle cell disease?
Current research suggests that CRISPR/Cas9 is a promising tool for correcting genetic diseases, including sickle cell. Safety is a paramount concern, and ongoing trials are monitoring for any potential adverse effects.
How far are we from a universally accessible cure?
Well, accessibility not only depends on the success of clinical trials but also on approval processes, cost, and healthcare infrastructure. It’s a big puzzle, but pieces are slowly falling into place.
What are the potential side effects of CRISPR/Cas9 treatment?
Like any medical treatment, CRISPR/Cas9 is not without risk. Potential side effects could include unintended mutations or immune reactions, but researchers are working to minimize these risks.
Can CRISPR/Cas9 be used to prevent sickle cell disease?
In theory, CRISPR/Cas9 could one day be used to repair mutations in embryos or gametes, thereby preventing the disease. However, that raises complex ethical questions that society must address.
I really hope that you’ve found this guide informative and that it helps you understand the potential of CRISPR/Cas9 gene editing for transforming the lives of those with sickle cell disease. Remember, science is constantly evolving, and what may seem like a distant possibility can quickly become reality with the right breakthroughs and support.
Founder, Rachele
(w) mybluegenes.com




One Comment